Your gut is one giant, mysterious, and microbe-laden lair.
If you consider the total bacteria in your gut compared to the number of cells in your body – the gut wins.
We are more bacteria than we are human.
Here’s the secret sauce…
If you figure out how to keep your microbes happy – you’ll keep the human side of you happy too.
In this rich gut ecosystem – bacteria have functions of their own.
The good guys produce byproducts like fuel and vitamins that our body finds useful; the bad guys produce byproducts and wastes that our body finds harmful.
More good guys = more good stuff. More bad guys = more bad stuff.
The bacteria self-regulate each other too.
The more diversity of bacteria you have in your body. The greater range of healthy byproducts you produce, pathogens you ward off, and metabolic stresses you sustain.
One of the top things that these microbes do for our body is maintain our gastrointestinal integrity.
Our gut is a “open” tube to the outside world – starting from our mouth, and ending at our bottom. It carefully lets digested nutrients in, and keeps the potentially harmful things out.
The gut is such an important interface between the “outside” and “inside” worlds – and its our bacterial friends – our gut flora – that help maintain and protect that barrier.
For my Game of Thrones fans, it’s like the Wall of the North. No one wants white-walkers or ice-breathing dragons across their gut wall.
Our microbes are like the Night’s Watch – they’ve sworn an oath to guard our gut day and night.
As a normal part of their lifecycle – bacteria die.
When certain types of bacteria die, they release components that are toxic to us. Specifically, they release Lipopolysaccharides (LPS). LPS are natural components of some bacteria membranes (even healthy ones). When the bacteria dies, the LPS is released.
As long as the gut is healthy – we handle just fine.
It’s when our guts are out-of-whack, the LPS leak into the bloodstream and wreak havoc throughout the body.
Research shows that just one single processed, high-fat and high-carbohydrate meal can increase the level of LPS in our bloodstream many-fold. LPS can remain elevated in the bloodstream over the course of weeks and months.
This state is called metabolic endotoxemia.
First, I’ll explain why metabolic endotoxemia is so worrisome (Ice dragons and White-Walkers aside) – and second, I’ll give you some strategies to deal with it.
Sound like a plan?
Let’s get to it.
Metabolic Endotoxemia
–Endo – Inside
-tox – Toxin
-emia – Blood
Endotoxemia is simply medical jargon for “toxins in the blood”.
The release of lipopolysaccharides (LPS) in the intestine is a normal feature of metabolism. It is abnormal when the LPS leaks into the bloodstream and triggers inflammation downstream.
The LPS becomes part of the outer membrane in “gram-negative” bacteria. “Gram positive” bacteria do not incorporate LPS into their membranes.
“Gram positive” and “gram negative” just refer to structural differences in bacterial membranes. When microbiologists view bacteria under a microscope, the outer membranes of gram-positive and gram-negative bacteria will “stain” differently when being plated for observation.
LPS in located in the outer membrane. When the bacteria die, this LPS component is released. A certain level of LPS release is normal.
If you consider that most Americans still have diets exceedingly low in food diversity and prebiotic starches and fibers from copious vegetables. The gut microbe environment can often become more tilted to LPS-containing bacteria.
If you have a healthy gut, there’s little to no trouble with LPS. If you have an inflammatory diet and unhealthy gut – LPS rises abnormally in the bloodstream and metabolic endotoxemia results.
Metabolic endotoxemia spikes and ebbs continuously over time – fueling inflammation that increases risk for chronic disease.
How High Lipopolysaccharides (LPS) Damage the Body
The release of LPS from bacteria in our gut starts with an inflammatory meal. An inflammatory meal leads to a chain of events that creates endotoxins and allows their release past the gut barrier.
When the gut barrier is weak or “leaky” or “permeable” – the endotoxins are able to migrate freely into the blood. Endotoxemia is a key feature of a disordered gut.
Once in the blood, LPS triggers a number of inflammatory events. LPS will interact with your fat cells and immune cells to create chronic inflammation in every tissue in the body. Recovery can take weeks and months.
Risks of metabolic endotoxemia stretch across body systems – and may set the stage for obesity, heart disease, autoimmunity, diarrhea, low sex hormones, and cognitive decline (such as Alzheimer’s disease).
This is why restoring gut health (and specifically the gut microbiome) is a central strategy to reducing risk for all of these diseases.
Negative Influence of Endotoxemia (LPS in the blood):
- Turns on inflammatory genes and strongly stimulates the release of inflammatory cell messengers. The cell messengers create a domino-effect of inflammation across the entire body including depression.
- Suppresses thyroid activity (1) & may promote autoimmune thyroid disease (2)
- Endotoxemia associated with markers seen in early Parkinson’s disease patients (3)
- Plays a role in triggering depression (4)
- Associated with Chronic Fatigue Syndrome (CFS) (5)
- Sets an inflammatory tone that initiates obesity, non-alcoholic fatty liver, and insulin resistance (6). Obese and insulin resistant states also lead to more inflammation and LPS release in the body.
It’s important to stop LPS in its tracks for all of these reasons!
How to Fix LPS Elevations in the Blood
Spore Probiotics:
The primary strategy to deal with endotoxemia is to support the integrity of the gut lining and gut mucosa.
Since spore probiotics are capable of surviving past the stomach acid in the gut, and play a central role in a healthy gut, they are my first line of defense when it comes to protecting from LPS.
An animal study found that Bacillus subtilis boosted the production of proteins necessary to help seal a damaged gut lining (7). B. subtilis has also been shown to help improve the absorptive area of the intestine (8) which is associated with reduced risk for inflammatory bowel diseases like Crohn’s, colitis, or celiac disease.
Other studies support the use of spore bacteria to reduce inflammation (9), increase the production of intestinal fuel, and increase levels of protective mucus.
A double-blind, placebo-controlled clinical study was recently conducted that examined the effect of spore probiotics (including Bacillus subtilis) on endotoxemia (10).
The participants were healthy and had low LPS in their blood to start. To trigger endotoxemia, the participants were given a McDonald’s breakfast to trigger leaky gut.
Here’s what the increase in endotoxins looked like following the challenge meal.
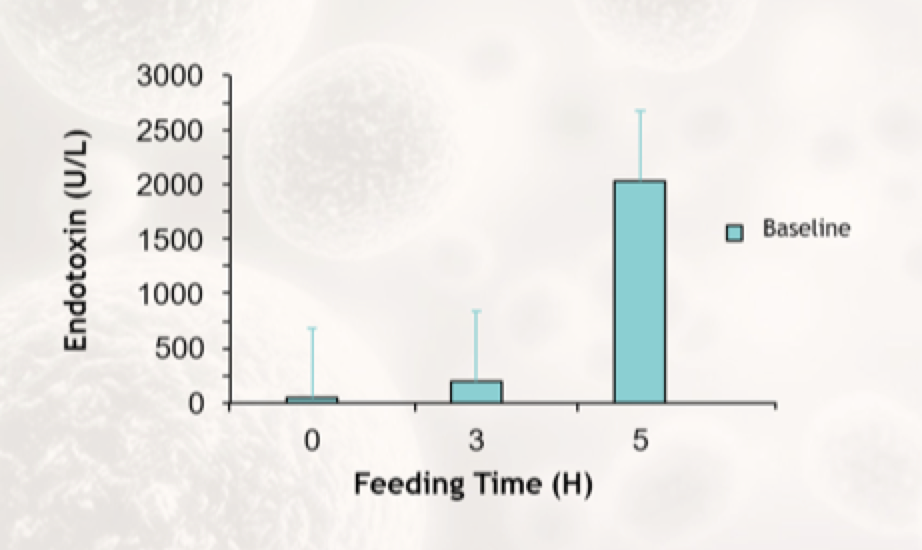 Endotoxin increase following challenge meal
Endotoxin increase following challenge meal
They were then supplemented with spore probiotics (Megaspore) over a period of 30 days.
In 30 days, the participants saw a 45% reduction in endotoxins in their blood. The placebo group saw a 32% increase!
The combined benefit (increase of endotoxin in placebo PLUS the % decrease in treatment group) was very large and may expand even greater if the study was conducted over a longer time period.
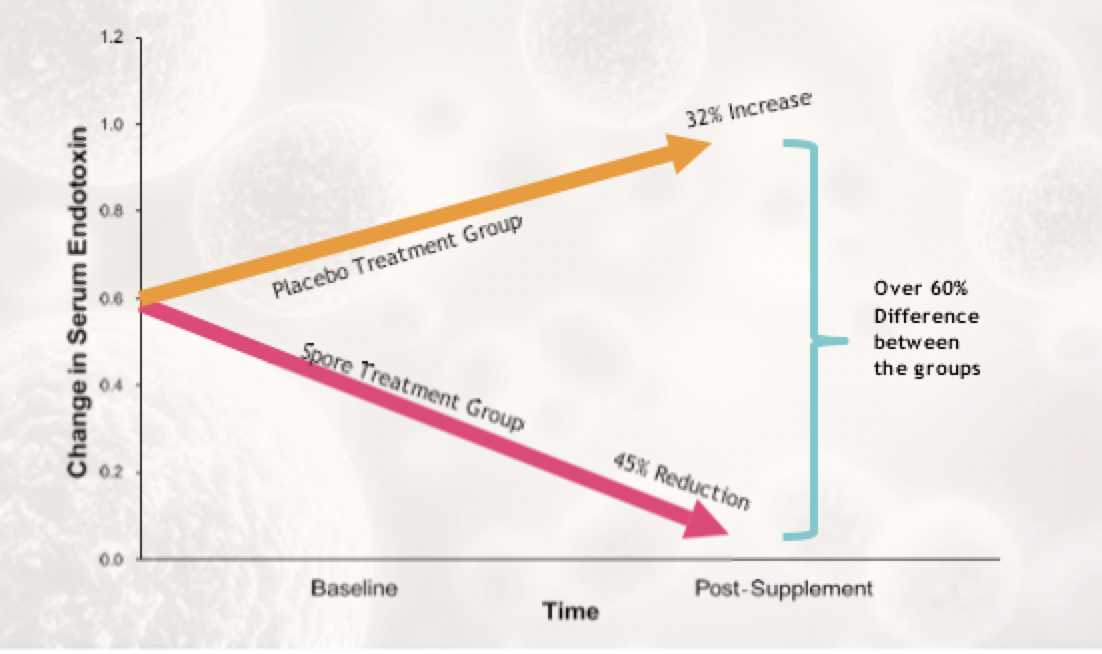 The improvement in endotoxin levels continued to expand between group receiving spore probiotics and the placebo as time progressed.
The improvement in endotoxin levels continued to expand between group receiving spore probiotics and the placebo as time progressed.
The study was continued for 90 total days. Over that time, triglyceride levels dropped just under 50mg/dL on average in the treatment group (remained the same in the placebo group).
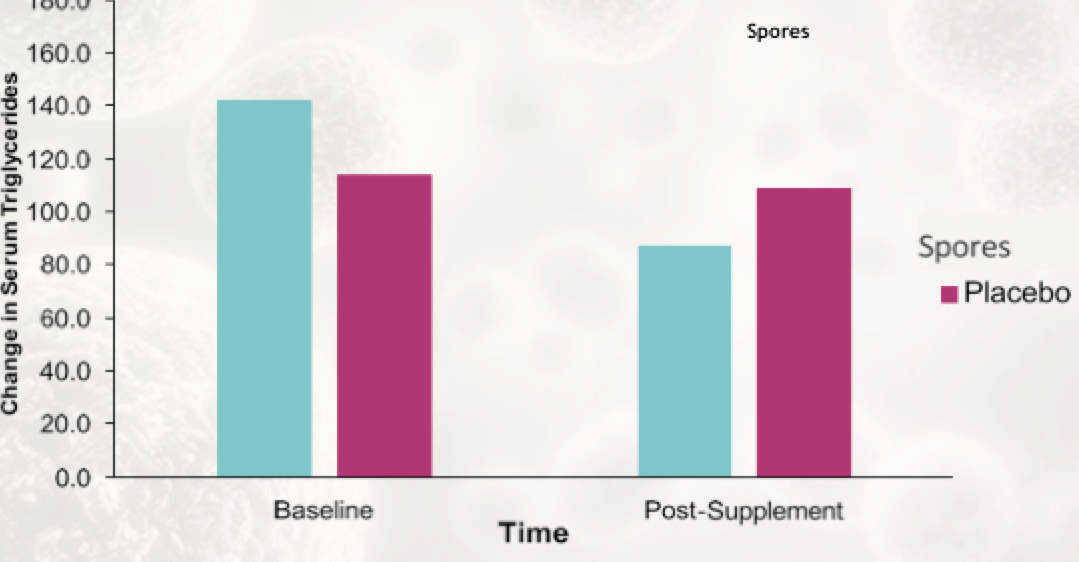 Participants receiving spore probiotics also saw reduction in blood triglycerides.
Participants receiving spore probiotics also saw reduction in blood triglycerides.
High triglyceride levels are also a general signal of metabolic endotoxemia.
Other markers improved such as inflammation (IFN-gamma), hunger (ghrelin) and blood sugar regulation (insulin; glucagon).
Elevated insulin & IFN-gamma are associated with high LPS leaking from the gut to the blood.
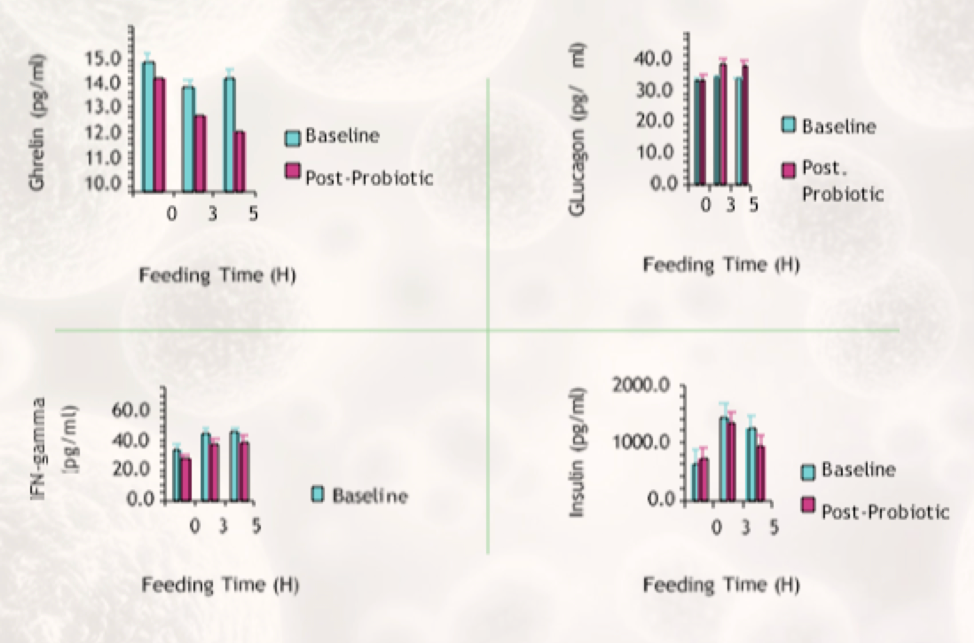 Markers for hunger (ghrelin), blood sugar (insulin and glucagon), and inflammation (IFN-gamma) improved in the treatment group.
Markers for hunger (ghrelin), blood sugar (insulin and glucagon), and inflammation (IFN-gamma) improved in the treatment group.
The researchers also measured MCP-1. MCP-1 is a general inflammatory immune marker that rises with inflammation and immune dys-regulation.
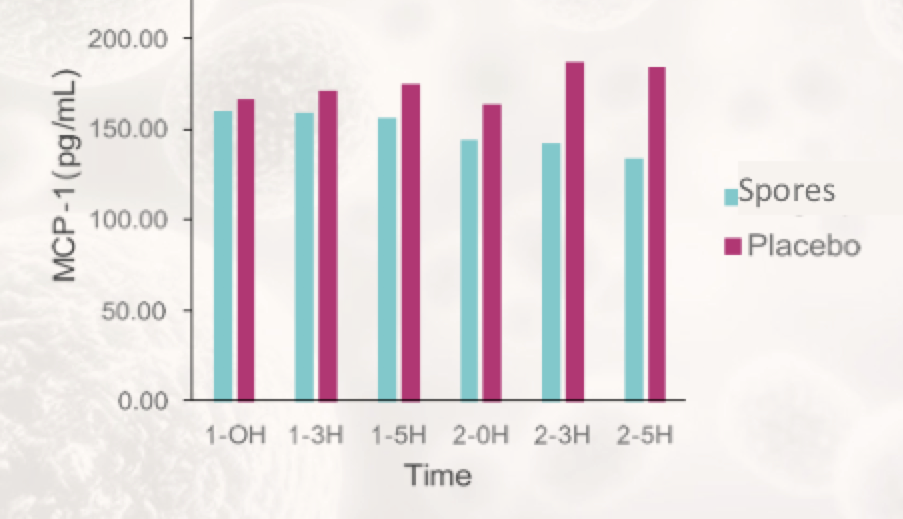 Inflammation & immune regulation (as measured by MCP-1) improved in probiotic group and generally worsened in the placebo group after a high-fat, high sugar challenge meal.
Inflammation & immune regulation (as measured by MCP-1) improved in probiotic group and generally worsened in the placebo group after a high-fat, high sugar challenge meal.
As a reminder, the study focused on healthy participants & did not focus on any other dietary changes or therapies. It just examined the effect of supplementation with spore probiotics. It is possible that the treatment findings may have been more profound if the participants’ guts were less healthy at the start.
Overall, in just 30 days of supplementation the participants receiving spore probiotics experienced reduction in immune dysregulation, inflammation, hunger, and endotoxins in the blood. They also demonstrated improvement in immune and blood sugar markers.
I personally use Megasporebiotic by Microbiome Labs as my preferred source of spore probiotics to support gut health.
Other Strategies to Heal Leaky Gut & Support Inflammation:
- Zinc Carnosine (directly heals mucosa)
- Lion’s Mane (supports nerve tissue healing and supports gastrointestinal integrity)
- MegaMucosa – contains a combination of LPS-binding immunoglobulins, anti-inflammatory bioflavonoids, and mucus-building amino acids. [MegaIgG2000 contains just the immunoglobulins – and can be used alonside Megamucosa.
- Curcumin (from Turmeric) (highly researched anti-inflammatory extract)
- L-Glutamine – supports a healthy GI lining and immune function.
- Prebiotics (feed good bacteria that then maintain the integrity of the gut lining & produce necessary fuel for bacteria and intestinal cells)
Related Articles:
- Can Elevated LDL Be a Protective Mechanism in Response to Inflammation and Leaky Gut?
- The Megasporebiotic Leaky Gut Clinical Trial
- Understanding Leaky Gut and Autoimmunity
- The 7 Core Strategies to Heal the Gut Lining and Manage Leaky Gut