The main thing when it comes to gut and immune health is to maintain the diversity of the gut microbiota.
This concept echoes Steven Covey’s mantra in
The Seven Habits of Highly Effective People:
“The main thing is to keep the main thing the main thing”.
The main thing that is consistent with IBS, Celiac disease, Crohn’s disease, Colorectal cancer, obesity, and general gut dysfunction – is a loss of microbiome diversity (1).
This article will help you “keep the main thing the main thing” & detail how to replenish diversity in a stepwise fashion to avoid the frustrating pitfalls of conventional advice.
The Microbiome – Your Internal Rainforest
High plant and animal diversity is a central feature of a healthy rainforest.
A rainforest is unique.
In a temperate forest, you can expect to find the same trees, plants, ferns, squirrels, and deer scattered uniformly across its miles.
Yet, in a rainforest, species are scattered in super diverse regional niches.
This “super-diversity” is what makes the rainforests the “lungs” of the world – breathing life to the earth & offering adaptability to change.
One might wipe out an entire species with the loss of only a small section of the whole. With each species loss, unique botanical remedies & cures can be lost too.
This makes a rainforest a perfect analogy for the diverse microbiota found in the regions of the gut.
Your gut is a rich ecosystem & a high level of diverse microbes is essential for it to function normally.
The gut delivers vital protective and sustaining roles for the entire body.
Lose a few key species and weeds and invasive predators can take over.
Protect the Gut Ecosystem by Protecting Diversity
An ecosystem model of gut function offers a sliding scale of gut dysfunction.
Important Note: A sliding scale spurs both proactive or reactive action – the model works the same whether you are sick currently or trying to ward off disease in the first place!
As we look at the chart below, symptom severity generally increases as you travel further to the right.
“Where” one falls on the scale does not necessarily correlate with the severity of symptoms experienced, nor with the “aggressiveness” of healing support needed to get the system back on track.
There’s always hope as one systematically protects the gut from losses and replenishes microbiome diversity & mucosal health.
Stages of Gut Dysfunction & Ecosystem Loss
A.) Digestive insufficiency, inflammation, dietary excess, & malnutrition promote swings in microbial diversity.
B.) As diversity falls, imbalance, “dysbiosis”, or leaky gut develops. “Endotoxemia” occurs as early as this stage.
C.) Dysbiosis is a state of relative overgrowth of bacteria or yeast. Lead to pH changes & less competition to crowd out opportunistic organisms.
D.) Overgrowth can become a clinical state such as small intestinal bowel overgrowth. Can contribute to more serious chronic complications.
E.) Overgrowth can become an infection with the threat of serious acute complications.
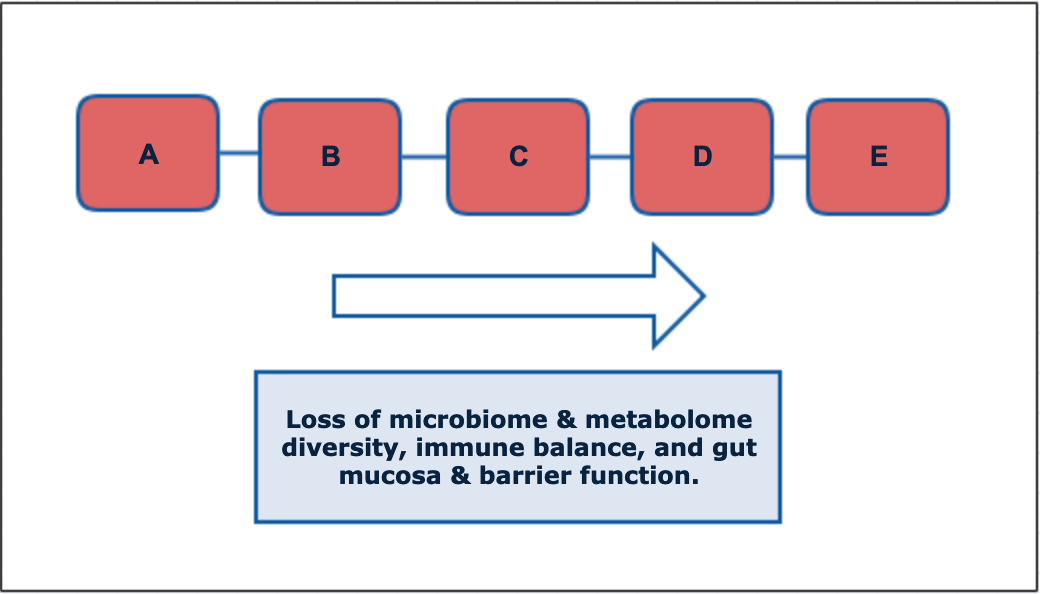
Recurring issues with bacteria or yeast overgrowth is a continued sign that diversity is low in the gut or that triggering factors are still driving imbalances.
Taking Probiotics to Restore Microbiome Diversity
Individual microbes that comprise the microbiome will differ between individuals – even if they share the same high level of diversity.
Efforts to replenish diversity with individual strains can be misguided.
The urge to find the exact strains to fit your exact health profile may be possible in the distant future – however, because healthy guts differ in their individual variation, current research teaches us that a focus on general groups & diversity of bacteria & yeast may be more beneficial than efforts to identify specific strain deficiencies.
The one thing that is consistent among healthy guts is high diversity, and likewise, among unhealthy guts is low diversity.
Taking Probiotics – Replenishing diversity in a stepwise fashion
- Address acute inflammation, digestive deficiencies, food triggers, infection, or mucosal repair.
- Add keystone microbes that are modulatory in nature.
- Introduce probiotics that are more stimulatory in nature.
- Titrate (start low and work up) an introduction of prebiotics to bolster diversity further & maintain diversity.
- Also titrate more complex dietary or supplementary prebiotics. Expand your diet to contain more diverse vegetables, rich in diverse starches, polyphenols, and phytochemicals.
- Reassess & decrease supplements as warranted.
- Continue proactive strategies based on personal tendency and/or genetic vulnerability.
*Along the way take a step back as needed to address overgrowth & infection, “die-off” from microbial death & rebalancing, inflammation & autoimmunity, food sensitivities/allergies/intolerances, digestive deficiencies, & mucosal maintenance & repair.
Problems with gut protocols are rooted in introducing a step too early or failing to address overgrowth, infection, die-off, inflammation, autoimmunity, food sensitivities/allergies, intolerances, digestive overwork and secretion deficiencies, & general mucosal repair.
A gut cannot be inflamed & rebuilding at the same time.
Definitions:
Probiotics – The World Health Organization defines probiotics as “live microorganisms, that, when administered in adequate amounts, confer a health benefit on the host”
Prebiotics – Starches, fibers, polyphenols, and phytochemicals that feed & maintain gut microorganisms.
Synbiotics – Probiotics and prebiotics taken together, especially when the prebiotic(s) selectively promote the included probiotic(s) – often leading to synergistic promotion of microorganism growth.
Microbiome / Microbiota – The combined microorganisms in a given environment (examples: gut, skin, oral, vaginal, whole body, soil). Interdependent with the state of the metabolome.
Metabolome – the combined metabolites, microbial byproducts, or physiologically active molecules in a given environment. Includes internally-derived & microbiome-derived metabolites. Interdependent with the state of the microbiome.
Dysbiosis – an imbalance of natural flora in the gut, commonly associated with chronic, low-level inflammation and leaky gut.
Overgrowth – A more pronounced imbalance of flora in the gut. Can be called an “infection”. Severity is “relative” in that it can lead to serious chronic health presentations, feed inflammation, autoimmunity, as well as disordered metabolism. Overgrowth may also set the stage for infection to occur. Involves otherwise healthy bacteria or yeast that is overgrown due to lack of competing organisms, excess fuel source (ex. sugar), or lack of diet diversity (less prebiotic fuel).
Infection – An overgrowth of an outside microbe, or a more acute overgrowth of a natural microbe, or growth of a microbe outside of its normal environment that is health-threatening. The “health-threatening” aspect can also apply to dysbiosis & overgrowth.
Triggers of Low Microbial Diversity in the Gut
If replenishing the microbiota is the goal – what causes a loss in microbial diversity?
Microbe diversity is lost from antibiotics, alcohol use, and consumption of inflammatory, allergic, sensitive, or intolerant foods.
Birth history, especially c-section delivery and formula feeding, also plays a large role in the development of flora diversity & may determine why one person needs more support than another.
Excess carbs and simple sugars combined with low diversity in starches, fibers, polyphenols, and phytochemicals from food is also a perfect recipe for low microbial diversity.
Stack those features together – and now you have a “perfect storm” for loss of microbial diversity in the gut.
Disruptions in gut function, topped with genetic vulnerabilities, can lead to a leaky gut, inflammation & widespread immune issues.
The Example of Wheat in the Diet
 Someone with a polymorphism in the HLA DQA2 or A8 genes will be more sensitive to proteins in wheat – but that genetic sensitivity may only be triggered if wheat is an early staple of your diet.
Someone with a polymorphism in the HLA DQA2 or A8 genes will be more sensitive to proteins in wheat – but that genetic sensitivity may only be triggered if wheat is an early staple of your diet.
These are easy to test with a cheek swab or blood test.
Because the circumstances vary per individual, it’s easy for the skeptics to cry that gluten-free diets are just another fad – while advocates cry that it’s the root cause of all of their health problems.
A healthy gut, in theory, should be able to tolerate some wheat in the diet – just not the gobs of it that are standard in first-world diets.
Wheat today is also very different from the wheat of yesterday – and the wheat in the United States is different from the wheat consumed in the European Union. You can say the same for wine & beer.
Many who travel abroad remark how they can tolerate many of the foods that would have them keeled over in discomfort in the US.
With diet diversity, sensitivities may just smolder under the surface & never kindle a raging fire of diagnosable Celiac disease – but certain gene combinations will increase the likelihood that wheat is a problem.
When the smoldering fire still causes problems but does not meet the standard medical criteria of “Celiac”, it is called “non-celiac gluten sensitivity (NCGS)“.
NCGS is associated with “extra-intestinal” (outside of the intestine) gluten symptoms where food sensitivity may cause neurological symptoms, brain fog, fatigue, joint pain, skin rashes, and other presentations without noticeable symptoms in the gut.
Standard medical practice only diagnoses celiac disease if you first test positive to one of two antibodies, and then follow with an intestinal biopsy to confirm damage to the small intestine.
The issue is that there are up to 24 antibodies related to wheat, not just the two related to gluten, which can be problems that can create immune sensitivities to wheat. You might test negative for the two most commonly measured, but be positive for one or more of the remaining 22 antibodies.
Additionally, damage to the intestines does not occur uniformly across the gut – it can occur in patches. The damage of celiac disease occurs microscopically. There’s a chance that they biopsy from a healthy part of the intestine & a diagnosis is missed despite the presence of positive antibodies.
Many with NCGS, or celiac disease go many years (or a lifetime) without being diagnosed.
From a 10,000-foot view, those carrying risk copies of the HLA genes are at higher risk of gluten sensitivity – and may proactively reduce or eliminate wheat in their diet so an antibody sensitivity or allergy is never triggered. Maintaining microbial diversity is much more important for these individuals.
This is just one snapshot of the dynamics behind diet diversity and genes.
A healthy gut can make you more tolerant to food that may be otherwise difficult to digest or bring your immune system on edge.
Maintaining the diversity of your gut microbiota is critical – it’s your blueprint to overcome any predilections you may have to food sensitivities, gut inflammation, or immune imbalances.
It’s also why so many people are failed by the conventional medical system that does not “recognize” why wheat may still be a problem with someone who does not have clinical Celiac.
The same story can connect to milk, corn, eggs, tree nut, or soy allergens. It can also apply to otherwise benign foods that you happen to have a heightened antibody response.
How do you maintain tolerance to these foods?
By supporting and sustaining microbial diversity in the gut!
In return, gut integrity is maintained.
We absolutely know that a healthy gut is diverse in gut microbes – and while the exact mix of microbes differs from person to person – there are general rules of thumb that we can follow to replenish and maintain diversity.
Reintroducing Diversity
 The most common probiotics include Lactobacilli, Bifidobacteria, Bacillus, & Saccharomyces bacteria.
The most common probiotics include Lactobacilli, Bifidobacteria, Bacillus, & Saccharomyces bacteria.
Others are important but are not stable enough to supplement orally.
You otherwise maintain these strains with prebiotic starches from the diet and supplements. Deficiencies in any one of these groups of flora will allow dysbiosis, overgrowth, or infection to develop.
A gut microbiome that lacks diversity – sets an environment where imbalances and overgrowths occur more easily – triggered at lower thresholds of insults than what may have been tolerated previously.
Promoting general groups of probiotics is often enough to shift the balance back in your favor and re-establish balance, pH, and higher diversity.
Small intestine bacteria (Lactobacilli) tend to be more immune-stimulating, and large intestine or colonic flora (Bifidobacteria) tend to be more immune balancing. I start with the balancing colonic flora and work my way up to more stimulating strains for this reason!
Lactobacilli focused probiotics may slow your efforts to replenish a loss of diversity (2). They are still important long-term but can be troublesome if introduced too early into a protocol.
Probiotic “Rule of Thumb”: Due to the immune-stimulatory nature of Lactobacilli probiotics, it is important to start with TrubifidoPRO foremost and introduce lactobacilli after other cornerstone bacteria have been replenished. You eventually need Lactobacilli too, yet they are commonly overgrown in the small intestine at the start of a gut protocol.
Prebiotic fibers and starches may feed wide groups of bacteria and potentiate any imbalance, so it’s important to reduce overgrowth and add immune-balancing bacteria foremost before promoting the growth of wide groups of bacteria with prebiotics.
We can also now be more selective with the prebiotic fibers we choose early on, and increase diversity as the microbiome allows.
If you have a poor response to a probiotic formulation – choose a more targeted formulation that has less risk of being too immune-stimulatory in the short-term.
Small intestine bacteria and (often Lactobacilli) bacteria will still be necessary long-term – but might be introduced too early or in too high of amounts that can be tolerated.
If there are immune imbalances – too strong of a stimulatory response can promote that imbalance more. Start with more modulatory focus later in the GI tract like a Bifidobacterium-rich probiotic, and add diversity from there.
Finally, introduce prebiotics in the form of supplements or foods in measured amounts that you can tolerate. I start with more targeted prebiotics like those found in MegaPrebiotic, and then progress to singular prebiotics such as partially hydrolyzed guar gum, and finally advance your intake with a broad spectrum prebiotic like FloraSpectrum Prebiotic Powder that contains inulin, arabinogalactins, and fructooligosaccharides.
To keep the gut guessing, I rotate probiotics and prebiotics every 1-2 months and routinely add new varieties of vegetables and fruits to my diet.
Here’s what a progression may look like for both Probiotics and Prebiotics based on the products I turn to foremost in my practice.
I start integrating prebiotics shortly after integrating Theralac. Like probiotics, taking prebiotics too early or too fast can set your gut protocol back in the short-term.
If you’re looking for a condensed version of a probiotic protocol using Microbiome Labs products – I encourage you to check out their Total Gut Restoration program. It is a great default program to follow – but I’ve included other probiotics and prebiotics that you can integrate.
Dr. Rinehart’s Stepwise Probiotic Progression:
1.) Megasporebiotic and TrubifidoPRO –
Provides spore probiotics and Bifidobacterium probiotics for early reconditioning of the flora. Megasporebiotic has been clinically studied to improve markers of leaky gut in as little as 30 days. The spores have also been clinically demonstrated to increase the diversity of other flora by 300-400%! For more spore diversity, I’ll use SporeBoost IG either alone or in conjunction with Megaspore. The added IgG helps support the binding of toxins released when crowding out unwanted microbes.
Start low and work your way up with Megasporebiotic due to its powerful reconditioning effects. You’ll help jumpstart metabolic activity, crowd out unwanted flora, and maintain your levels of spore probiotics as part of the microbe diversity in your gut.
TrubifidoPRO is a Bifidobacteria-focused probiotic that is delivered safely through the stomach acid due to a unique patented capsule process that uses sodium alginate – an algae-derived compound that delivers the probiotic strains in a trojan horse fashion.
TrubifidoPRO features a unique probiotic delivery process that delivers the probiotics safely to the gut past stomach acid and bile acids early in the digestive process – something that you will not see with other probiotics, including those in a delayed-release capsule.
2.) Megasporebiotic and Theralac –
In this stage, Theralac is integrated as a substitute for TrubifidoPRO. Prior to trying Theralac, I usually have clients taking Bifidospectrum. Theralac starts introducing some Lactobacilli strains, but is balanced with Bifidobacteria strains as well. It’s my preferred broad-spectrum probiotic of Lactobacilli and Bifidobacteria strains.
I’ll introduce Theralac by taking it in the morning, and still take TrubifidoPRO at night before switching to Theralac twice a day. The goal is to take Theralac in the morning and again at night for more advanced support – many see benefits at once a day.
If you’re looking for my wellness recommendation for good probiotics to take, it is the combination of these two formulas!
For kids or those looking to avoid capsules, Master Supplements’ Granular Theralac is a powder form of Theralac that can sprinkled and “folded” into applesauce, yogurt, and other foods. The granules are not intended to be blended as you’ll lose the acid-proof delivery. Simply spoon it in to your food or beverage.
Alternatively, Spore probiotics are very stable at high heat and capsules can be opened up and mixed and blended directly in food and beverages.
3.) Periodically Rotate in TruFlora –
TruFlora is a Lactobacilli-focused group of probiotic strains that is great at immune-stimulation and cleansing. I integrate it last as it is immune stimulating. I take it on trips with me for extra support, and may also turn to it in a more dedicated detoxification phase of my diet and lifestyle.
I tend to switch between Theralac, and TrubifidoPRO monthly. Every 5th month or so, I will integrate TruFlora. This keeps my system guessing and helps support flora diversity which is the primary goal.
You can also do these products in combination, but for practicality & to keep my system guessing – I focus on one product at a time unless I’m following a special protocol.
4.) Acute & Targeted Probiotic Support –
If I suspect yeast overgrowth or need higher levels of support, I’ll add Restorflora and/or HU58. These are particularly useful in C diff protocols and Candida-balancing protocols for the additional targeted support they provide.
Bonus Discussion: Butyrate acts as fuel for the colon and immune cells – and a deficiency is correlated with a host of digestive maladies. I’ll use Sunbutyrate TG by Pure Encapsulations to support supplemental intake while you wait for gut rebalancing to produce ample amounts on its own. TrubifidoPRO and processing of some polyphenols like those in PhytoFlora Microbiome Support naturally support the production of Butyrate and short-chain fatty acids too!
Butyrate is a “metabolite” of healthy probiotics and a staple component of a healthy “metabolome” (see definitions above). It supports the health of colon cells, maintenance of the mucosal lining, and immune function. Some butyrate-producing bacteria are unstable in the presence of oxygen – so typical capsules will not work. Microbiome Labs has developed a novel encapsulation process & capsule delivery to create an air-tight capsule in an oxygen-free laboratory environment that does not open until in the oxygen-free regions of the gut.
A diverse metabolome is as important as a diverse microbiome – and both work together to in a virtuous cycle. Butyrate is a keystone component of a healthy metabolome – and now we can support it in ways not thought possible until now.
Prebiotic fibers, starches, and supplements also promote Butyrate as they can feed some of these special butyrate-producing bacteria that normally cannot be supplemented orally.
Read on to learn how to ease prebiotics into your protocol…
Dr. Rinehart’s Stepwise Prebiotic Progression
While you can introduce precision prebiotics early on in a protocol, I like to wait at least 3-5 weeks (21-35 days) prior to introducing any prebiotic formula. This minimum delay allows some microbial rebalancing to occur and prepares the gut for more support.
For me, this normally happens 2-3 weeks after first introducing Theralac to a protocol (step 2 in the Probiotic progression above).
Start low with a quarter of the intake and work your way up to tolerance. If it’s still too much, look back to your probiotic progression or check out the 7 Core Strategies article to see where your missing links may be.
1.) MegaPrebiotic – A Precision Prebiotic:
Megaprebiotic contains three unique branched fiber compounds that selectively feed keystone groups of bacteria that are consistent among healthy guts.
Megaprebiotic preferentially promotes these strains before promoting wider strains with other prebiotic types. These keystone bacteria include Akkermansia muciniphila, Faecalibacterium prausnitzii, and Bifidobacteria.
2.) Partially Hydrolyzed Guar Gum (Sunfiber):
Partially hydrolyzed guar gum (PHGG) is a unique prebiotic that has been shown to help with both diarrhea-dominant and constipation-dominant irritable bowel syndrome.
Our preference is to start with
This is because TruFiber does have a little bit of inulin that may add too much complexity early on in gut protocols.
Sunfiber only contains PHGG, so it’s less likely to run into potential issues with inulin.
Inulin is a great prebiotic, it promotes a wider swath of bacteria that may not be preferred early in a protocol.
Trufiber is a great bridge between Sunfiber and our next recommendation.
The small amount of inulin in Trufiber is not inherently bad, but may be “too much too soon” for sensitive individuals.
Using a product like Trufiber can help prepare your body to higher-dose inulin and other prebiotics like those found in the next recommendation.
And so you might introduce them in that order (1. Sunfiber Powder, 2. then TruFiber, then branch into diverse prebiotics like those found in the next section).
PHGG in the products above is a great first-line choice for those who do not like the stevia sweetness found in MegaPrebiotic.
PHGG is tasteless and is easily added to food and drink. Always start low and work up with any prebiotic.
3.) Inulin, Larch arabinogalactans, and FructoOligoSaccharides (FloraSpectrum Prebiotic Powder):
These prebiotic fibers work together to promote a wider swath of beneficial flora in the gut. I like to wait until I’ve promoted more balance in the microbiome prior to adding FloraSpectrum so that it is better tolerated.
If FloraSpectrum is too much, go back to TruFiber. If Trufiber is an issue, go back to FloraStart, and if that’s an issue, go back to Megaprebiotic!
If you have trouble tolerating any prebiotic, check out my discussion on the 7 core strategies to heal the gut lining…you may benefit from a different strategy such as focusing on probiotic strategies, fine-tuning the diet, directly targeting bacterial overgrowth, or supporting sources of inflammation more directly.
4.) Rotate and Try Others! (Above formulations, PhytoFlora Microbiome Support, & others like Poly-Prebiotic Powder by Pure Encapsulations)
PhytoFlora Microbiome Support contains polyphenols which have recently been demonstrated to have prebiotic properties in addition to anti-inflammatory and antioxidant benefits.
Once you’ve worked your way through these products, now it’s time to mix and match and rotate them to keep your system guessing. The body craves diversity, and giving it unique starches and fibers on a rotating basis will do the trick.
Check out the Prebiotic Diversity Trio when you’re ready for this step. It contains 1 bottle each of Sunfiber, FloraSpectrum, and PhytoFlora at bundled pricing.
Prebiotics can come from diet foremost, but most Americans will benefit from a rotating supply of prebiotic supplements.
Long-Term: Daily Wellness Intake of Probiotics and Prebiotics
Long-Term Probiotic Schedule:
1.) Megasporebiotic at 3 days on 7 Days Off, 2 capsules a day after a meal. Can rotate SporeBoost IG as an alternative or take 1 capsule of SporeBoost IG and 1 capsule of Megasporebiotic to promote ultimate spore diversity.
2.) TrubifidoPRO and Theralac every other month, TruFlora every 5th month, 1 capsule a day after meal
3.) Targeted Support as needed: RestorFlora, Hu58, Sunbutyrate TG
Long-Term Prebiotic Schedule:
1.) Megaprebiotic is a foundational formula for precisional support of keystone flora, 1 scoop a day will do it!
2.) Mix and match Sunfiber, TruFiber, FloraSpectrum, PhytoFlora Microbiome Support, and others! You can rotate products similar to probiotics, but you can also separate them by time of day, ex/ Sunfiber in the morning, and MegaPrebiotic at night. Or 1/2 a serving of products at the same time. Make it your own. Check out the Prebiotic Diversity Trio to jumpstart your mix & match plan.
3.) Continuously add new varieties of vegetables in your diet! This is what the body intended aside from supplements. Try different colored carrots & cauliflower. Try unique vegetables at an ethnic food store. Eat lots of greens, and try the bitter ones too! Eat a different root vegetable each day like rutabaga, turnip, beets, parsnips, kohlrabi, and all of the colors in between.
Taking Probiotics in Step-Wise Fashion:
- Think of the Total Gut Restoration protocol as scaffolding for your gut repair – and the additional probiotics and prebiotics as a way to get even more rounded support.
- Check out my 7 Core Strategies to Heal the Gut Lining and Manage Leaky Gut which has received more excitement and positive feedback than any other article I’ve written to this date. Check this out especially if you have trouble tolerating new products.
- Between the Total Gut Restoration Protocol, the 7 Core Strategies, and the Probiotic and Prebiotic progressions described above, you will have a very complete picture of how to personalize your own strategy.
- For acute replenishing following antibiotic therapy – check out What Probiotics Should be Taken With or After Antibiotic Treatment
- Honorable Mention to Spore Probiotics: The Megasporebiotic Recurrent C Diff Study
- For acute replenishing following antibiotic therapy – check out What Probiotics Should be Taken With or After Antibiotic Treatment
- If at any point your symptoms flare abruptly, lower intake levels or simply revert back to a previous stage of your progression where you were tolerating the products!
While there is always a place for professional coaching to guide you through a protocol, these discussions will save you research and hopefully answer a lot of questions for you along the way.
There’s a LOT of secret sauce in this discussion. I hope you enjoyed and please take a moment to share the article and submit your email for more content like this!





