A little-known secret about LDLs or “bad cholesterol” is that their levels in the blood can serve as a marker for inflammation in the body.
LDLs are carriers of fat, and so more or less fat intake will call for more or fewer LDLs to shuttle them around the body.
Research has not shown decreasing LDLs to be correlated with reduced cardiovascular mortality, however.
As fat intake and cholesterol are only part of the story, could inflammation be the missing link?
High LDL levels do not reflect only fat intake, high levels can also reflect high inflammation.
LDLs will also increase in response to inflammation as they are able to bind and neutralize toxins – an overlooked, yet vital role for LLs in the body.
It’s been reported in the literature for over three decades that LDLs can serve as antibacterial compounds that bind endotoxins – making them less dangerous and preventing the activation of an immune response. Immune responses to LPS can be 20 to 1000-fold less severe when LPS is able to bind to LDL (1; 2; 3; 4; 5; 6; 7; 8; 9; 10).
 Both LDL and HDL may be protective against inflammation by binding toxins in the bloodstream. Excess may be more indicative of inflammation from a number of sources, including a leaky gut. Instead of cholesterol, should we be focused on inflammation instead?
Both LDL and HDL may be protective against inflammation by binding toxins in the bloodstream. Excess may be more indicative of inflammation from a number of sources, including a leaky gut. Instead of cholesterol, should we be focused on inflammation instead?
This is game-changing in our understanding of why cholesterol levels are linked with heart disease – yet also why our cholesterol-lowering strategies over previous decades have missed the mark.
This protective effect of lipids on LPS and immune activation may partly explain why low cholesterol and LDL levels are correlated with an increase in all-cause mortality (11; 12; 13; 14).
High levels of LDL and cholesterol may still be associated with health issues because of the toxicity they may reflect – not because of inherent harmfulness independent of context.
Instead of focusing on the cholesterol levels themselves – perhaps instead we should be focused on the reasons for elevations in endotoxins.
Where do chronic high levels of endotoxins come from?
A leaky gut.
Where Inflammation Begins in the Body
Inflammation is the body’s healing response. It is the process by which the body brings immune cells and healing components to an injured or infected area.
Normally, the inflammation does the dirty work and then patches things up and resolves so that the immune system and body can calm down and focus on the next task.
Inflammation, even at low levels, can cause disease when it becomes chronic. The inflammatory process gets “stuck’ and sometimes needs some coaxing to help rebalance and calm down.
Inflammation Stems from Three major sources.
1.) Trauma – physical, chemical, emotional, or infectious.
2.) Overconsumption of omega-6 fatty acids and insufficiency of omega-3 fatty acids.
3.) Leakiness of the gut that allows pathogens, toxins, and poorly digested food proteins to absorb into the blood and trigger inflammation throughout the body.
1.) Physical, chemical, emotional, or infectious trauma
This type of inflammation is easier to understand. If you bump your head it swells up, gets red and warm, and hurts. Inflammation in this context is easy to understand.
If you breathe in a toxin, eat a pesticide, or apply man-made chemicals to the skin – the body responds to it in similar ways.
This is not as easy to understand as the bump on the head – and as such, is more problematic when it comes to the long-term risk of chronic disease stemming from chronic inflammation.
Emotional trauma is also difficult to “see”, but chemically it is very real and can affect our immune reactivity, stress response, pain threshold, and more.
If you have an infection, inflammation and LPS levels can peak in a short period of time.
Alcohol and sugar are also examples of compounds that directly irritate all cells and tissues of the body – causing oxidative stress and inflammation.
2.) Ratio of Omega-6 and Omega-3 Fats

Omega-6 and omega-3 fats are found in the oils of plants and animals.
They are predominant in sunflower, safflower, grapeseed, soybean, corn, cottonseed, and canola oil among others.
Omega-3 fats are found in fish, nuts, algae, and precursors can be found in plants such as flax.
Omega-6 fats serve as precursors to inflammatory molecules used by the body. The more omega-6 fats that are available – the more inflammation that can be produced.
When omega-6-rich oils are purified, they are also naturally unstable because of their “unsaturated” chemical structure.
Unsaturated fats are prone to oxidation – a process by which fat becomes the cellular equivalent of a “ricocheting bullet”.
Saturated fats are not prone to oxidation (less likely to become a ricocheting bullet in the body) and are otherwise stable for use in cooking and baking.
Saturated fats may not be the enemy after all. They may ultimately be protective of heart disease risk. Excess intake of carbohydrates, omega-6 fats, and other sources of inflammation such as endotoxins from a leaky gut may be more strongly linked with cardiovascular risk than saturated fat intake.
Normally, some omega-6 fat intake is healthy and essential – at least when balanced by anti-inflammatory omega-3 fats.
Omega-3 fats play important roles in healthy cell structure and communication, mood, immunity, gut mucosal health, and the gut microbiome.
Diets high in omega-6-rich oils are inflammatory. Ideally, diets should contain a ratio of omega-6 and omega-3 fats of 2:1 or even 1:1.
Instead, the American dietary ratio ranges anywhere from 10-100:1. The ratio is 500%-10,000% higher than it should be!
Removing omega-6-rich seed oils from the diet is one of the most powerful things you can do to reduce the omega-6:omega-3 ratio and reduce oxidative stress in the body – two major mechanisms of inflammation in the body.
In return, heart disease risk declines.
The other way to manage omega-6:omega-3 balance is to increase omega-3 fat intake through intake of fish, algae, supplements, and some plants.
I discussed the important roles of the omega-3 fats EPA, DHA, and DPA when it comes to inflammation and the microbiome in a recent article: Discover the Role of Omega-3 Fats for the Microbiome.
Omega-3 fats help to decrease inflammation, counterbalance excess omega-6, have targeted mechanisms to support gut health and the microbiome, along with maintaining brain, mood, immune, and cellular health.
Omega-3 fatty acids also are metabolized into specialized pro-resolving mediators (SPMs, PRMs) that help to finish and complete the inflammatory process. You can support PRM/SPM production by consuming omega-3 fats or taking these omega-3 derivatives as supplements.
Omega Complete by Doctor Alex Supplements contains high levels of DHA, EPA, and DPA. MegaOmega by Microbiome Labs contains EPA, DHA, and DPA, along with added pro-resolving mediators to support normal omega-3 levels and inflammation.
3.) Leaky Gut and Inflammation
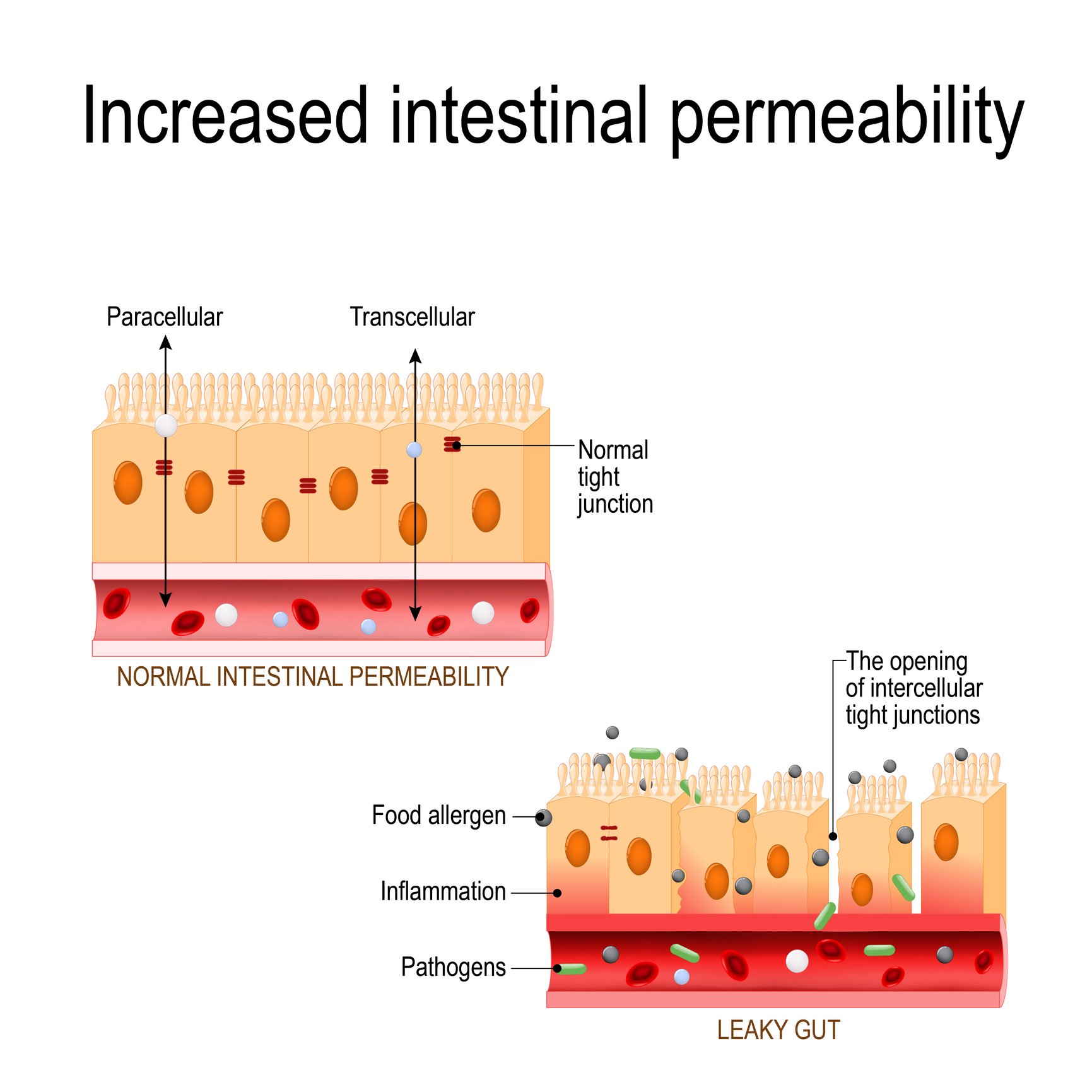
A leaky gut is demonstrated by larger gaps between the tight cells that line the gut – allowing allergenic proteins, pathogens, and toxins to find their way into the blood.
In order to link the effect of fat on the diet and heart risk, it’s necessary to talk about the gut – and specifically the absorption of lipopolysaccharides (LPS) from an unhealthy gut.
LPS are endotoxins that come from dying bacteria in our gut. LPS are a component of the cell membrane of gram-negative bacteria (such as E. coli).
When bacteria die in the course of a natural life cycle, their cell membrane structure is broken up. LPS that was once a part of the cell membrane is now released into the gut.
When the gut lining is “leaky”, this inflammatory LPS is readily absorbed into the blood through micro-holes in the barrier.
When LPS migrates into the bloodstream at a greater rate than our normal defenses can keep up with, it is known as “metabolic endotoxemia“.
Endotoxemia causes inflammation throughout the body and is a major link behind all chronic diseases.
If you ever heard of “sepsis” – a major cause (or end-stage) of death – it is caused by endotoxins completely overwhelming our body’s defenses.
Yet, you do not need LPS to be at “sepsis” levels for the endotoxins to be a problem.
It only takes low levels of endotoxins acting over months, years, and decades to contribute to the incidence of chronic disease, including brain-degenerative processes, diabetes, and immune over-activation.
The promotion of a healthy gut barrier and support of a healthy gut microbiome naturally prevents the ability of endotoxins to build up in the blood.
A lowered ability for LPS to find its way into the bloodstream is one of the most powerful and proactive strategies for whole-body wellness.
Inflammation is a primary driver of all chronic diseases. Omega-6 fat intake, insufficient omega-3 intake, and endotoxemia from LPS are predominant causes of inflammation.
Strategies to Support Leaky Gut and Endotoxemia
1.) Remove allergic, sensitive, and leaky-gut-causing foods, often including wheat, other grains, dairy, corn, soy, and eggs.
Some of these foods can be healthy but are often consumed in unnaturally high frequency. Frequent exposure to any food can lead to sensitivity.
Wheat is especially problematic because we do not produce the enzymes necessary to fully digest it (even if we do not have an immune allergy or sensitivity to wheat).
This means that EVERYONE, without exception, experiences a leaky gut after consuming wheat.
A leaky gut can be likened to the presence of micro-tears in the lining of the gut. The lining normally protects what gets into the blood and what stays out.
When the tears occur in a fashion that is greater than the body’s ability to repair – large proteins and toxins are able to get into the bloodstream – triggering immune reactions and inflammation throughout the body.
The “tears” in the lining set the stage for endotoxemia and immune sensitivities. This process of “leaky gut” is also believed to be a necessary component of ALL autoimmune diseases (15).
Remember, excess sugar and alcohol intake may also contribute to a leaky gut.
For a more comprehensive step-by-step approach to healing the gut lining and managing leaky gut, check out one of the most popular blog articles: The 7 Core Strategies to Heal Leaky Gut.
2.) Consider taking supplemental immunoglobulins.
Immunoglobulins or IgG are proteins found in milk that help bind up toxins and support mucosal health. Serum-derived IgG avoids issues with allergenic proteins that may otherwise be found in cow milk.
I use IgG-Boost 2500 by Doctor Alex Supplements (powder), Mega IgG2000 by Microbiome Labs (capsules), and also use MegaMucosa by the same company as my preferred sources of IgG. They are suitable for individuals with milk allergies or sensitivities but are not suitable for those with a beef allergy.
Berries contain proanthocyanidins as active antioxidant compounds that may also support the binding of LPS (16).
A supplement such as Pro-Antho Forte by Progressive Labs may also support the intake of proanthocyanidins while also supporting gut health and inflammation.
3.) Support inflammation naturally.
I use substances such as curcumin or omega-3 fatty acids often to support inflammation.
Theracurmin HP by Integrative Therapeutics is arguably the most well-absorbed form of curcumin at the time of this writing.
For omega-3 support, I use Omega Complete DHA, EPA, and DPA Support or other fish oil supplements to support inflammation.
I like the MegaOmega formulation as it preferentially targets the ratios of omega-3 fats associated with gut mucosa and microbiome health.
Omega-3 fats are well-regarded to support healthy cholesterol and lipid values in addition to their anti-inflammatory properties.
A number of extracts can serve anti-inflammatory purposes – bromelain and systemic enzymes, ginger, PEA, Vitamin D, and licorice flavonoids may all support inflammation, in addition to curcumin which is my favorite catch-all.
For support of brain inflammation, I like gingko which is often combined with other herbs. I also Lion’s mane mushroom to support cognition, gut, and nerve health. For cognitive support, I use Brain Fog Support which contains an extract backed by 5 human clinical trials examining outcomes for stress, memory, and more.
Regular movement, alongside a strength-training and flexibility routine, will also do wonders to support inflammation naturally – while also reducing the stress…
4.) Stress support is also globally supportive of your body’s immune health, metabolism, resilience to inflammation, as well as the maintenance of a healthy stomach and gut lining.
The most comprehensive adaptogenic mix I have seen is Qualia Mind – caffeine-free. Other very popular stress support supplements include Everyday Stress Support, Cortisol Manager and HPA Adapt by Integrative Therapeutics, or Mycobotanicals Stress Decompress, or Suntheanine.
For sleep support, ProSom by Integrative Therapeutics is an excellent and somewhat perfect formulation as it combines magnolia (found in Cortisol Manager), magnesium, theracurmin, and L-theanine. Unlike many sleep supplements, ProSom does not contain melatonin.
When turning to melatonin, I use a 0.3mg Herbatonin by Symphony Natural Health.
Melatonin is also anti-inflammatory, especially for the brain. I reserve Herbatonin for nights where I really need to be on-point the next morning or following travel across time zones. I always have a box of Herbatonin in my pantry for these purposes and one box lasts a while with sporadic use.
Anti-inflammatory diets and lifestyle strategies should also not be overlooked for stress balance as diet and environmental toxins can be sources of physiological stress.
5.) Address Overlooked Diet and Lifestyle Factors for Inflammation and Oxidative Stress
- Overeating (one of my favorite proactive strategies is intermittent fasting)
- High intake of unstable fats (reduce omega-6 oils)
- Consuming more than 1-2 glasses of alcohol (and recent evidence suggests that one can still be too much)
- Smoking
- Poor dental hygiene (your oral bacteria can “seed” the gut in good and bad ways, you swallow millions of bacteria with each drop of saliva. Consider Biocidin Throat spray to support the balance of oral bacteria,
Practice normal brushing and flossing. Remove added sugars from diet and beverages.Dental health is a MAJOR contributor to inflammation and heart disease risk.
- Overeating (one of my favorite proactive strategies is intermittent fasting)
- Eating allergic/sensitive/intolerant foods – especially wheat, and often cow milk products.
- High intake of simple sugars and carbohydrates. These fuel sources are not as clean and their metabolism can be “messy” in terms of the oxidative stress produced.
- Taking medications with side effects that may increase blood sugar, slow liver metabolism, or cause oxidative stress due to inherent toxicity.
- Eating allergic/sensitive/intolerant foods – especially wheat, and often cow milk products.
6.) Diet and Supplement Approaches to Metabolic Stress
Here are some of my favorite strategies to counterbalance metabolic stress from inflammation and overeating:
- One of the best emerging strategies is to use a new form of niacin (Vitamin B3) called nicotinamide riboside (NR) – known commercially as TruNiagen.NR is known for supporting NAD+ levels and for supporting the expression of an anti-aging group of genes known as sirtuins, specifically SIRT2.NAD+ is referred to as the “central regulator of metabolism”. It’s important for healthy cellular activity and metabolism is in line with ATP.Like ATP, life is not possible without NAD+. NAD+ declines with age and with metabolic stress.For more on NR and anti-aging, check out my article “Fountain of Youth” Benefits of Nicotinamide Riboside – a New Form of Vitamin B3
- Non-flush niacin is more affordable and may work well enough for cholesterol support purposes.
- NMN powder like that found in With-N by Renovovita also supports NAD+ levels. Yet contains one of the best formulas for the cost that I am aware of with CoQ10, activated B Vitamins, and PQQ.
- Resveratrol helps protect the body from oxidative stress and to trick the body to think it is in a fasting state by turning on fasting-related genes. It may also work synergistically with the NR found in Truniagen. I will also use a liposomal form of trans-resveratrol. Resveratrol was one of the first substances to make headlines in the anti-aging world. It is still at the forefront of healthy aging strategies. Daily Phyto Balance contains curcumin, resveratrol, and other highly researched botanicals that support inflammation.
- Intermittent fasting deserves another mention as it improves your metabolic efficiency during the block of hours that you are eating, and, fasting doesn’t require an outside supplement or expense to implement in your lifestyle.To optimize my metabolism, I use Truniagen PRO 500mg, Resvero XL and a 16:8 intermittent fasting schedule.
- One of the best emerging strategies is to use a new form of niacin (Vitamin B3) called nicotinamide riboside (NR) – known commercially as TruNiagen.NR is known for supporting NAD+ levels and for supporting the expression of an anti-aging group of genes known as sirtuins, specifically SIRT2.NAD+ is referred to as the “central regulator of metabolism”. It’s important for healthy cellular activity and metabolism is in line with ATP.Like ATP, life is not possible without NAD+. NAD+ declines with age and with metabolic stress.For more on NR and anti-aging, check out my article “Fountain of Youth” Benefits of Nicotinamide Riboside – a New Form of Vitamin B3
7.) Support the Gut Microbiome with Probiotics and Prebiotics.
Megasporebiotic is our most popular probiotic, and the number one product sold on our store.
- It has been shown by clinical trial to reduce leaky gut (as measured by endotoxin levels) in as little as 30 days.
- It also has recently been clinically shown to reduce triglycerides significantly over a 6-12 week period.
Other sources of probiotics and prebiotics are also important. I carry another set of spore probiotics for diversity in SporeBoost IG. I use BifidoSpectrum Probiotic initially and, after some time, will introduce TheralacPRO as my preferred full-spectrum probiotic. These are taken in addition to Megasporebiotic.
I also use prebiotics to support synergy with the probiotics – but also to help maintain the diversity of strains that may not be available as oral supplements. Prebiotics are nature’s means of supporting good bacteria in the gut – so the goal is to incorporate as many unique prebiotics into your diet as well.
Supplementally, I introduce prebiotics in the following order, personalizing as I need. Megaprebiotic, FloraStart Prebiotic Fiber, Trufiber, and FloraSpectrum Prebiotic Fiber.
Long-term, I mix and match this prebiotics to add diversity and variety. Unsure of your gut diversity? You can measure using a test like BiomeFx.
While protocols may begin by limiting prebiotics in the diet, eventually they should be added back in slowly as the gut allows.
Remember to incorporate dietary prebiotics regularly. Most leafy greens and diverse vegetables and fruits have prebiotic properties. Adding new and diverse sources is essential for healthy gut maintenance.
Examples of High Prebiotic Foods:
- Onions, garlic, leeks, jicama, green bananas, sunchokes (Jerusalem artichokes), asparagus or radish have some of the highest prebiotic content.
- Root vegetables like parsnips, beets, celery root, rutabega, turnips, kohlrabi, or daikon.
- Blackberries, raspberries, strawberries and more.
- Eat a variety of greens from kale, spinach, collard greens, swiss chard, arugula, and many others.
These foods provide non-digestible starch and help add bulk to stool for optimal transit time through the gut.
If you don’t love the taste, hide some of these foods in smoothies and mix with other things that you do like. I recommend smoothies over juices, as juices concentrate the sugars and otherwise take away the valuable fiber.
I’ve discussed my probiotic strategy in depth in other resources such as my Probiotic Blueprint, and have summarized a number of articles on our Taking Probiotics page.
Related Articles:
- Revisiting the Diet-Heart Hypothesis
- Support Immunity Naturally with these 10 Foundational Strategies
- Is Saturated Fat Healthy?
- The Megasporebiotic and Triglycerides Study
- The Megasporebiotic Leaky Gut Clinical Trial
- Understanding Leaky Gut and Autoimmunity
- How to Stop Your Gut from Leaking Toxins into Your Blood: A Closer Look at Metabolic Endotoxemia and Spore Probiotics
- Does Leaky Gut Exist?





