Millions suffer from daily bloating and digestive discomfort.
They seek advice with mixed results.
While I have found identifying and removing food sensitivities such as gluten and dairy helps in significant ways – it can be a starting point as bacterial overgrowth, bloating, and distention can linger despite “eating all the right things”.
Removal of food sensitivities is just one step of the conversation – reconditioning the microbiome is the long-term goal for most gut conditions.
Treating the double-edged sword of FODMAPS with reverence and care is an important piece of a gut restoration formula that can surely make the difference between success and failure.
FODMAPs refer to Fermentable Oligosaccharides, Disaccharides, Monosaccharides, And Polyols.
A healthy functioning microbiome breaks down “FODMAP” compounds with ease – moreover, the compounds fuel activity and maintain the growth of healthy bacteria.
If you overwhelm your microbiome’s capacity to break down components of food OR if you have the wrong balance of otherwise healthy bacteria in the gut – bloating and inflammation can occur.
Gas, after all, is a byproduct of fermentation.
If the microbiome is out of balance – most commonly seen as small intestinal bacterial overgrowth (SIBO) or in the context of chronic inflammation – even normal levels of FODMAPs will cause problems.
So if you or someone close to you has ever had gut symptoms triggered by seemingly benign foods like dairy, apples, blackberries, cauliflower, tomatoes, beans, lentils, artichokes, mangos, asparagus, Brussels sprouts, squash, honey, onions, garlic, and many grains, chances are this article is for you.
I’ve detailed the 7 main phases in my most popular article: The 7 Core Strategies to Health the Gut Lining and Manage Leaky Gut.
Elimination of food allergy, sensitivity, and intolerance triggers is only one of the strategies.
As you might expect, it’s not the full story.
Knowing when to handle FODMAP-containing foods carefully can be a difference-maker in cases that do not respond to conventional elimination diets.
FODMAPS and the Gut Microbiome
The microbiome is the total number and balance of healthy microbiota living in your intestinal tract.
These friendly bugs influence inflammation, mood, nutrient status, and immune health.
Keeping them happy (or helping them become happy again) is a target of many of the protocols I use with clients and the basis of most of the strategies I share.
The microbiome produces numerous metabolites that the body uses to respond to its environment and function optimally.
Individual metabolites from bacteria in the gut are known as “postbiotics”. The sum total of these metabolites and postbiotics is referred to as the “metabolome”.
Arguably, the “metabolome” is the ultimate goal of a healthy functioning gut, as its role is to extract as many nutrients and beneficial compounds without inflicting collateral damage to our body during the process.
If I had a “food pyramid approach” to wellness, boosting the health of the gut microbiome (and the total “metabolome” as a result) would be at the base of the pyramid alongside stress management and blood sugar regulation.
These are my “three amigos” of wellness.
Fermentable means that bacteria act on a compound, similar to brewer’s yeast’s ability to turn sugar into alcohol. It also means Candida albicans can convert dietary sugars to alcohol – contributing to similar stresses of alcohol consumption – without the need for alcohol consumption in the first place!
If a microbe can ferment a substance, it is also using that substance as a fuel.
Eat the wrong things, and you will fuel the growth of the wrong bacteria – leading to the wrong postbiotics and metabolites circulating in the body.
It’s a matter of time before an inadequate diet triggers adverse symptoms.
Saccharides make up a large portion of FODMAPS.
These are various types of starches and sugar connected in “chains” that require further action to be broken down into usable form by the body.
Bacteria provide that “further action.”
With the exception of sugar alcohols like sorbitol or xylitol (under the “polyol” category in FODMAPs), complex sugars promote the growth of gut flora.
Sugar alcohols are not able to be broken down, and as such create inflammation, water retention, and discomfort in the GI tract.
They are also known to disturb the balance of healthy gut flora as the ecosystem doesn’t know what to do with them.
Sugar substitutes such as sucralose, aspartame, and saccharin have similar adverse effects.
Despite being non-caloric, these sugars are associated with weight gain and not loss, most likely due to unwanted changes in the microbiome.
I’ve discussed a landmark study recently that emphasizes the links between a healthy gut microbiome and weight management. I’ve also talked about why you should avoid sugar substitutes.
Excess, or eating too much of limited forms of saccharides, can overwhelm our body’s fermentation capacity or over-promote certain types of bacteria and yeast over time.
Low-FODMAP Diet and Long-term Gut Health
FODMAPs are normally healthy compounds for the gut.
They act as prebiotics, promoting the growth of beneficial bacteria, and they maintain levels of these organisms over time.
When imbalances arise due to antibiotics, excessive alcohol use, a carbohydrate-rich diet, food sensitivities, and processed foods, even healthy bacterial species become overgrown.
Overgrowth most commonly occurs in the small intestine.
The small intestine is long but small in diameter. It typically has bacterial levels an order of magnitude lower than those of the large intestine (colon), where most fermentation occurs.
When you have extra fermentation happening in the small bowel – in an area not used to that level of bacteria growth – discomfort is an understandable result.
FODMAP consumption – in the context of small bowel overgrowth – potentiates the imbalance even though it’s usually a healthy thing to do.
Consider a low-FODMAP diet as a SIBO treatment strategy.
The Wrinkles of a Low-FODMAP Diet
I’ve detailed the ins and outs of a Low-FODMAP diet in the past, and I’ll summarize here.
Many foods contain FODMAP compounds. Counterintuitively – many of these foods are largely considered healthy in the grand scheme of diverse fruits, vegetables, roots, and tubers.
Here are the most common high and moderate-FODMAP containing foods:
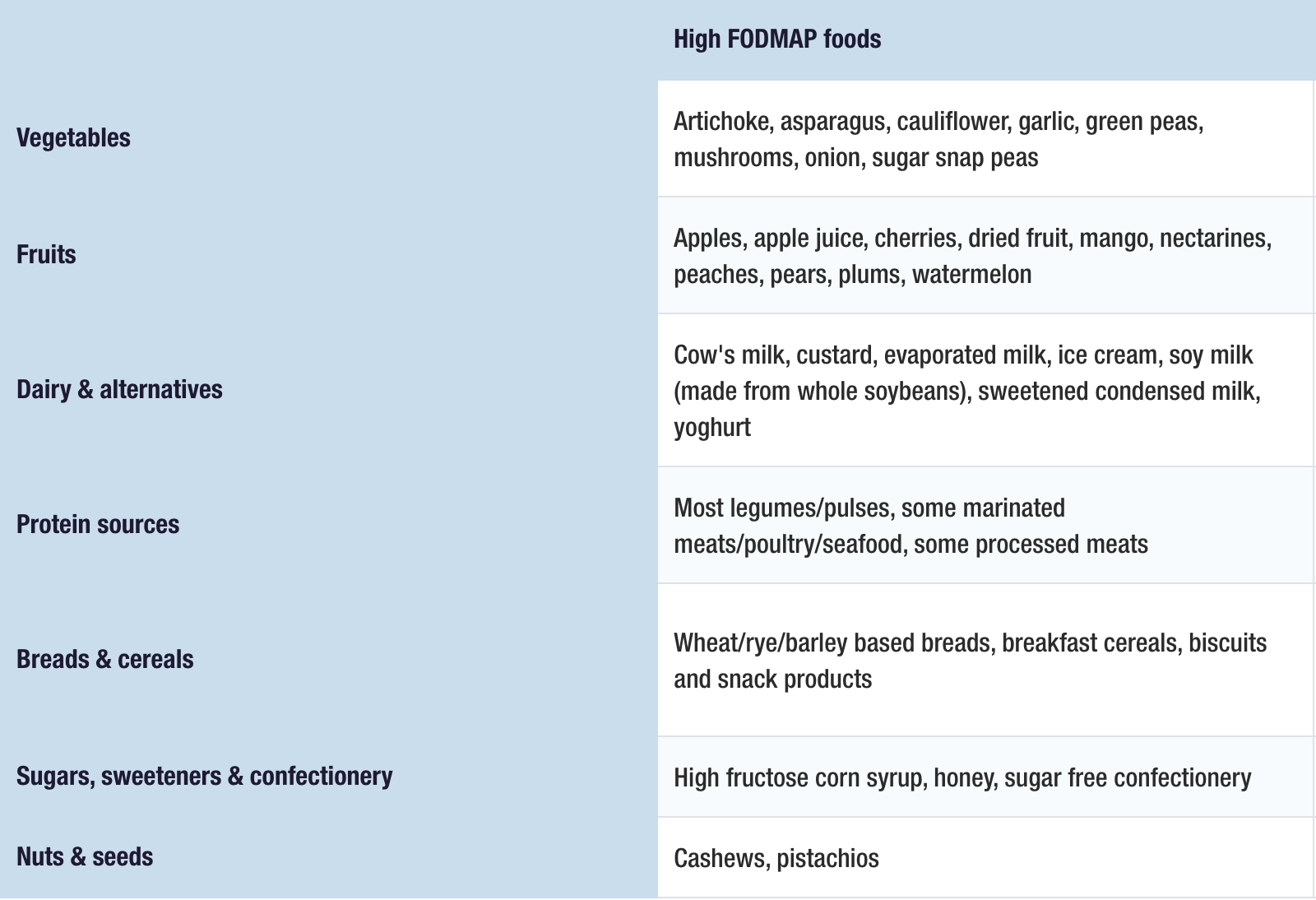
Image source: https://www.monashfodmap.com/about-fodmap-and-ibs/
As discussed above, in the context of an out-of-balance microbiome known as “dysbiosis” – FODMAPs may actually do more to potentiate the imbalance than they do to promote healthy bacteria in the first place.
This is the basis of the “Catch-22” with FODMAP consumption (and supplements).
The other side of that sword is that FODMAPs are also absolutely necessary to maintain an otherwise healthy microbiome.
A low-FODMAP diet may be necessary to clear the slate in the short term, yet it is ultimately intended to be a short-term strategy.
This is why it’s a “low” FODMAP diet and not a “No” FODMAP diet. FODMAPs are normal and wanted aspects of a healthy diet.
The biggest mistake of a “low FODMAP” diet is treating it as a long-term strategy beyond a reasonable 1-3 month period, sometimes 4-6 months.
A long-term FODMAP diet unnecessarily starves WANTED bacteria in the gut – and can lead to species and diversity loss – despite superficial improvements in bloating, discomfort, and distention.
It is a penultimate example of the balancing act of removing FODMAPs completely for a short period, then slowly reintroducing them one by one as the system allows.
In the interim, many strategies exist to re-establish the gut microbiome so that it can handle these compounds comfortably. While many truly depend on an individualized approach, I’ve parsed them more directly in some of my more popular articles:
The emphasis in each article is a step-by-step or phase-by-phase approach to healing the gut and to introducing a diversity of foods (and/or measured doses of supplements).
Everyone is different as to which FODMAP foods they can introduce first, how quickly, and the many forks in the road one may need to take to tolerate more.
The answer to which FODMAPs to introduce and when is to reintroduce one food at a time, generally every four days.
The ultimate goal is to re-establish the level and diversity of the gut microbiome by working with what you have to optimize gut function.
FODMAPs also work in an additive effect – meaning that an individual food may not trigger symptoms – but if you eat a lot of it (like a whole canister of hummus) – or if you combine a lot of separate high-FODMAP foods – you may trigger a ‘breaking point” where you’ve overwhelmed your system’s capacity to break down the FODMAP-containing foods.
The ultimate strategy can split hairs to the point where green lentils are okay, yet red lentils send you running to the bathroom. Or, a tablespoon of hummus with cucumber is fantastic, yet the 2nd tablespoon has you feeling like a blueberry blimp exemplified by Violet Beauregarde in Willy Wonka.
Luckily, when in doubt, a new tool now exists to help you digest FODMAPs in foods and help you succeed more completely in the “low-FODMAP” portion of your protocol.
This tool is an adjunct – not a solution. And it’s there to buy time until you fully recondition the gut and reestablish a well-functioning gut microbiome.
The product is FODMATE by Microbiome Labs. It contains the exact enzymes your body needs to break down FODMAPs while following a low-FODMAP diet plan.
You will still want to introduce targeted, precision prebiotics and evolve your protocol as your diet and system allows. Yet FODMATE is an absolute game-changer when it comes to the toleration of an already limited diet plan.
My hope with this discussion is that you take a titrated approach as your system allows and you place setbacks as part of the process and not as a complete failure of an otherwise thought-out plan.
FODMATE can help stem the tide while you go through the more difficult changes of a gut-restoration plan. For more dietary instruction check out our Low-FODMAP diet resource and/or work with a local functional medicine professional familiar with your case.
It will not digest sugar alcohols, the P in FODMAPs known as polyols. These should be limited in the diet, preferably <2 g/day, but optimally 0 g/day. In the “2010’s”, there was a lot of excitement about the possibilities of sugar alcohols before the research caught up.
As a result, there are some otherwise good supplement formulas that unfortunately contain sugar alcohols as flavor enhancers that may or may not trigger problems. I’m careful not to throw the baby out with the bathwater, and to find alternatives when they exist. They can be benign in the 1-2 gram sugar alcohol range, but when used as ice cream sweeteners and more – they’re more of a nuisance than a benefit.
Research is revealing that even small dietary changes can have a dramatic effect on the gut microbiome.
Equipped with the discussion and resources of the article, you can confidently navigate when to push forward, and when to pull back.
Most importantly you can connect the dots and context as to why some approaches succeeded, and others failed.
FODMAPS are finicky factors to a healthy diet – yet now I hope you now have an understanding, resources, and blueprint for dealing with them optimally. In the meantime, a new FODMAP enzyme supplement can help you while following a low-FODMAP portion of your diet protocol.
Related Articles:




